World Journal of Emergency Medicine ›› 2014, Vol. 5 ›› Issue (4): 270-274.doi: 10.5847/wjem.j.issn.1920-8642.2014.04.005
• Original Articles • Previous Articles Next Articles
Toru Hifumi1( ), Ichiro Okada2, Nobuaki Kiriu2, Eiju Hasegawa2, Tomoko Ogasawara2, Hiroshi Kato2, Yuichi Koido2, Junichi Inoue3, Yuko Abe1, Kenya Kawakita1, Masanobu Hagiike1, Yasuhiro Kuroda1
), Ichiro Okada2, Nobuaki Kiriu2, Eiju Hasegawa2, Tomoko Ogasawara2, Hiroshi Kato2, Yuichi Koido2, Junichi Inoue3, Yuko Abe1, Kenya Kawakita1, Masanobu Hagiike1, Yasuhiro Kuroda1
Received:2014-05-20
Accepted:2014-10-09
Online:2014-12-15
Published:2014-12-15
Contact:
Toru Hifumi
E-mail:hifumitoru@gmail.com
Toru Hifumi, Ichiro Okada, Nobuaki Kiriu, Eiju Hasegawa, Tomoko Ogasawara, Hiroshi Kato, Yuichi Koido, Junichi Inoue, Yuko Abe, Kenya Kawakita, Masanobu Hagiike, Yasuhiro Kuroda. Thyroid hormone alterations in trauma patients requiring massive transfusion: An observational study[J]. World Journal of Emergency Medicine, 2014, 5(4): 270-274.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn//EN/10.5847/wjem.j.issn.1920-8642.2014.04.005
Table 1
Baseline characteristics for the massive transfusion and control groups
| Variables | Massive transfusion (n=19) | Controls (n=19) | P value |
|---|---|---|---|
| Age (yr) | 44.4±23.2 | 57.2±24.5 | 0.12 |
| Gender, male, n (%) | 17 (89.4) | 15 (78.9) | 0.30 |
| Mechanism of injury Penetrating/Blunt | 2/17 | 0/19 | 0.16 |
| Interval between injury and admission (min) | 47.2±21.8 | 51.5±13.9 | 0.49 |
| ISS | 30.7±2.9 | 16.0±2.9 | <0.01 |
| Lactate (mmol/L) | 3.0±1.7 | 2.6± 2.4 | 0.62 |
| SBP (mmHg) | 102.0±30.0 | 130.6±28.8 | <0.01 |
Table 2
Comparison of the 24-hour transfusion requirements, specific therapeutic interventions, and outcomes between the massive transfusion and control groups
| Variables | Massive transfusion (n=19) | Controls (n=19) | P value |
|---|---|---|---|
| Transfusion required within 24 h: RCC (U) | 19.3±8.8 | 0.8±2.1 | <0.01 |
| FFP (U) | 18.7±9.5 | 1.1±2.9 | <0.01 |
| PC (U) | 13.5±11.7 | 0 | <0.01 |
| Calcium administration (for the first seven days, mg) | 4247±3038 | 141± 601 | <0.01 |
| Catecholamine administration, n (%) | 0 (0) | 0 (0) | |
| Glucocorticoid administration, n (%) | 3 (15.8) | 2 (10.5) | 0.65 |
| Insulin administration, n (%) | 0 (0) | 0 (0) | |
| Mortality within 28 days, n (%) | 0 (0) | 1 (5.3) | 0.47 |
| Mortality during hospitalization, n (%) | 0 (0) | 1 (5.3) | 0.47 |
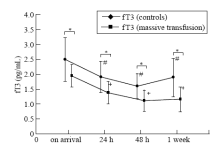
Figure 1.
Serial changes in free triiodothyronine at different sampling times in the 2 groups (mean±standard deviation). *P<0.05 compared with the control group; #P<0.05 compared with data at admission in the control group; +P<0.05 compared with data at admission in the massive transfusion group. Shaded area represents normal free triiodothyronine reference range.
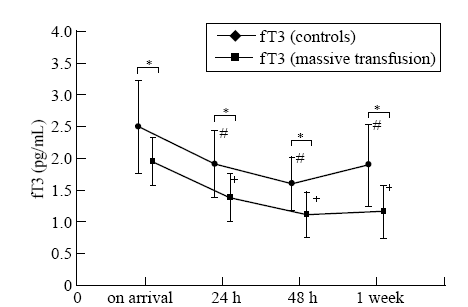
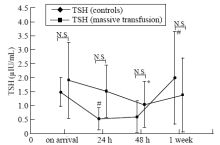
Figure 3.
Serial changes in thyroid stimulating hormone levels at different sampling times in the 2 groups (mean±standard deviation). #P<0.05 compared with data at admission in the control group; +P <0.05 compared with data at admission in the massive transfusion group. Shaded area represents normal TSH reference range.

| 1 | Warner MH, Beckett GJ. Mechanisms behind the non-thyroidal illness syndrome: an update.[J]. Endocrinol. 2010; 205:1-13. |
| 2 |
Scoscia E, Baglioni S, Eslami A, Iervasi G, Monti S, Todisco T. Low triiodothyronine (T3) state: a predictor of outcome in respiratory failure? Results of a clinical pilot study. Eur J Endocrinol 2004; 151:557-560.
doi: 10.1530/eje.0.1510557 pmid: 15538932 |
| 3 |
Hamilton MA, Stevenson LW, Luu M, Walden JA. Altered thyroid hormone metabolism in advanced heart failure. J Am Coll Cardiol 1990; 16:91-95.
doi: 10.1016/0735-1097(90)90462-x pmid: 2358611 |
| 4 |
Sawin CT, Chopra D, Albano J, Azizi F. The free triiodothyronine (T3) index. Ann Intern Med 1978; 88:474-477.
pmid: 637426 |
| 5 |
Rink C, Siersleben U, Haerting J, Mende T, Nilius R. Development of the low-T3-syndrome and prognosis assessment in patients with liver cirrhosis. Gastroenterol J 1991; 51:138-141.
pmid: 1811659 |
| 6 |
Borkowski J, Siemiatkowski A, Wolczynski S, Czaban SL, Jedynak M. Assessment of the release of thyroid hormones in septic shock—prognostic significance. Pol Merkur Lekarski 2005; 18:45-48
pmid: 15859546 |
| 7 |
Girvent M, Maestro S, Hernández R, Carajol I, Monné J, Sancho JJ, et al. Euthyroid sick syndrome, associated endocrine abnormalities, and outcome in elderly patients undergoing emergency operation. Surgery 1998; 123:560-567.
pmid: 9591009 |
| 8 |
Gou DY, Su W, Shao YC, Lu YL. Euthyroid sick syndrome in trauma patients with severe inflammatory response syndrome. Chin J Traumatol 2006; 9:115-117.
pmid: 16533439 |
| 9 | Phillips RH, Valente WA, Caplan ES, Connor TB, Wiswell JG. Circulating thyroid hormone changes in acute trauma: prognostic implications for clinical outcome. J Ttrauma 1984; 24:116-119. |
| 10 |
Aun F, Medeiros-Neto GA, Younes RN, Birolini D, de Oliveira MR, The effect of major trauma on the pathways of thyroid hormone metabolism. J Trauma 1983; 23:1048-1051.
doi: 10.1097/00005373-198312000-00005 pmid: 6655750 |
| 11 |
Grill E, Strong M, Sonnad SS, Sarani B, Pascual J, Collins H, et al. Altered thyroid function in severely injured patients. J Surg Res 2013; 179:132-137.
doi: 10.1016/j.jss.2012.09.008 pmid: 23043865 |
| 12 |
Facktor MA, Mayor GH, Nachreiner RF, D'Alecy LG. Thyroid hormone loss and replacement during resuscitation from cardiac arrest in dogs. Resuscitation 1993; 26:141-162.
doi: 10.1016/0300-9572(93)90174-o pmid: 8290809 |
| 13 |
Dulchavsky SA, Lucas CE, Ledgerwood AM, Grabow D, Brown TR, Bagchi N. Triiodothyronine (T3) improves cardiovascular function during hemorrhagic shock. Circ Shock 1993; 39:68-73.
pmid: 8481977 |
| 14 |
Vitek V, Shatney CH. Thyroid hormone alterations in patients with shock and injury. Injury 1987; 18:336-341.
doi: 10.1016/0020-1383(87)90056-8 pmid: 3508880 |
| 15 | Hoffenberg R, Ramsden DB. The transport of thyroid hormones. Clin Sci (Lond) 1983; 65:337-342. |
| 16 |
Hamblin PS, Dyer SA, Mohr VS, Le Grand BA, Lim CF, Tuxen DV, et al. Relationship between thyrotropin and thyroxine changes during recovery from severe hypothyroxinemia of critical illness. J Clin Endocrinol Metab 1986; 62:717-722.
doi: 10.1210/jcem-62-4-717 pmid: 3949952 |
| 17 |
Vitek V, Shatney CH, Lang DJ, Cowley RA. Thyroid hormone responses in hemorrhagic shock: study in dogs and preliminary findings in humans. Surgery 1983; 93:768-777.
pmid: 6857495 |
| 18 |
Sterling K, Brenner MA, Sakurada T. Rapid effect of triiodothyronine on the mitochondrial pathway in rat liver in vivo. Science 1980; 210:340-342.
doi: 10.1126/science.7423197 pmid: 7423197 |
| 19 |
Shigematsu H, Smith RA, Shatney CH. Triiodothyronine increases survival in canine hemorrhagic shock. Resuscitation 1987; 15:233-243.
doi: 10.1016/0300-9572(87)90002-5 pmid: 2831596 |
| 20 |
Yuan XQ, Shatney CH, Dewitt DS, Prough DS, Smith RA. Triiodothyronine (T3) antagonizes adverse effects of high circulating reverse-T3 (rT3) during hemorrhagic shock. Am Surg 1988; 54:720-725.
pmid: 3195847 |
| [1] | Gui-long Feng, Miao-miao Zheng, Shi-hong Yao, Yin-qi Li, Shao-jun Zhang, Wei-jing Wen, Kai Fan, Jia-li Zhang, Xiao Zhang. Risk factors and predictive model of adrenocortical insufficiency in patients with traumatic brain injury [J]. World Journal of Emergency Medicine, 2021, 12(3): 179-184. |
| [2] | Yong Liang, Hong Zeng, Yu-geng Liu, Ai-min Xu, Wen-hong Liu. Prevalence of post-traumatic stress disorder after earthquakes among the elderly in China: A meta-analysis [J]. World Journal of Emergency Medicine, 2021, 12(2): 137-142. |
| [3] | Samantha Shwe, Lauren Witchey, Shadi Lahham, Ethan Kunstadt, Inna Shniter, John C. Fox. Retrospective analysis of eFAST ultrasounds performed on trauma activations at an academic level-1 trauma center [J]. World Journal of Emergency Medicine, 2020, 11(1): 12-17. |
| [4] | Linda C. Chokotho, Wakisa Mulwafu, Mulinda Nyirenda, Foster J. Mbomuwa, Hemant G. Pandit, Grace Le, Christopher Lavy. Establishment of trauma registry at Queen Elizabeth Central Hospital (QECH), Blantyre, Malawi and mapping of high risk geographic areas for trauma [J]. World Journal of Emergency Medicine, 2019, 10(1): 33-41. |
| [5] | Hojat Sheikh Motahar Vahedi, Hadi Hajebi, Elnaz Vahidi, Amir Nejati, Morteza Saeedi. Comparison between intravenous morphine versus fentanyl in acute pain relief in drug abusers with acute limb traumatic injury [J]. World Journal of Emergency Medicine, 2019, 10(1): 27-32. |
| [6] | Bianca M. Wahlen, Ayman El-Menyar, Mohammad Asim, Hassan Al-Thani. Rapid sequence induction (RSI) in trauma patients: Insights from healthcare providers [J]. World Journal of Emergency Medicine, 2019, 10(1): 19-26. |
| [7] | Brian G. Cornelius, Elizabeth Webb, Angela Cornelius, Kenneth W.G. Smith, Srdan Ristic, Jay Jain, Urska Cvek, Marjan Trutschl. Effect of sedative agent selection on morbidity, mortality and length of stay in patients with increase in intracranial pressure [J]. World Journal of Emergency Medicine, 2018, 9(4): 256-261. |
| [8] | Suresh Kumar Arumugam, Insolvisagan Mudali, Gustav Strandvik, Ayman El-Menyar, Ammar Al-Hassani, Hassan Al-Thani. Risk factors for ventilator-associated pneumonia in trauma patients: A descriptive analysis [J]. World Journal of Emergency Medicine, 2018, 9(3): 203-210. |
| [9] | Ahmed El Muntasar, Ethan Toner, Oddai A. Alkhazaaleh, Danaradja Arumugam, Nikhil Shah, Shahab Hajibandeh, Shahin Hajibandeh. Effect of angioembolisation versus surgical packing on mortality in traumatic pelvic haemorrhage: A systematic review and meta-analysis [J]. World Journal of Emergency Medicine, 2018, 9(2): 85-92. |
| [10] | Saeed Mahmood, Omaima Mahmood, Ayman El-Menyar, Mohammad Asim, Hassan Al-Thani. Predisposing factors, clinical assessment, management and outcomes of agitation in the trauma intensive care unit [J]. World Journal of Emergency Medicine, 2018, 9(2): 105-112. |
| [11] | Kasim Turgut, Mehmet Ediz Sarihan, Cemil Colak, Taner Güven, Ali Gür, Sükrü Gürbüz. Falls from height: A retrospective analysis [J]. World Journal of Emergency Medicine, 2018, 9(1): 46-50. |
| [12] | Salima Kerai, Omrana Pasha, Uzma Khan, Muhammad Islam, Nargis Asad, Junaid Razzak. Association of post-traumatic stress disorder and work performance: A survey from an emergency medical service, Karachi, Pakistan [J]. World Journal of Emergency Medicine, 2017, 8(3): 214-222. |
| [13] | Pothiawala Sohil, Pua Yong Hao, Leong Mark. Potential impact of early physiotherapy in the emergency department for non-traumatic neck and back pain [J]. World Journal of Emergency Medicine, 2017, 8(2): 110-115. |
| [14] | Ruo Wu, Luo-gen Peng, Hui-min Zhao. Diverse coagulopathies in a rabbit model with different abdominal injuries [J]. World Journal of Emergency Medicine, 2017, 8(2): 141-147. |
| [15] | Changiz Gholipour, Bahram Samadi Rad, Samad Shams Vahdati, Amir Ghaffarzad, Armita Masoud. Evaluation of preventable trauma death in emergency department of Imam Reza hospital [J]. World Journal of Emergency Medicine, 2016, 7(2): 135-137. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
