World Journal of Emergency Medicine ›› 2021, Vol. 12 ›› Issue (3): 207-213.doi: 10.5847/wjem.j.1920-8642.2021.03.008
• Original Articles • Previous Articles Next Articles
Yu-qing Cui1, Xian-fei Ding1, Huo-yan Liang1, Dong Wang1, Xiao-juan Zhang1, Li-feng Li2, Quan-cheng Kan3, Le-xin Wang4, Tong-wen Sun1( )
)
Received:2020-05-29
Accepted:2021-01-21
Online:2021-06-01
Published:2021-05-31
Contact:
Tong-wen Sun
E-mail:suntongwen@163.com
Yu-qing Cui, Xian-fei Ding, Huo-yan Liang, Dong Wang, Xiao-juan Zhang, Li-feng Li, Quan-cheng Kan, Le-xin Wang, Tong-wen Sun. Efficacy and safety of low-dose corticosteroids for acute respiratory distress syndrome: A systematic review and meta-analysis[J]. World Journal of Emergency Medicine, 2021, 12(3): 207-213.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn/EN/10.5847/wjem.j.1920-8642.2021.03.008
Table 1
Summary of identified RCT studies
| Study | Country | Center | Number of patients | Female/ male | Age, years (mean±SD) | Initial daily dosea | Time of treatment initiation | Duration of treatment (days) | Primary outcome | Secondary outcomes | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mortality | MV free days (mean±SD) | New infection rate | ||||||||||||||
| SG | NG | SG | NG | SG | NG | SG | NG | SG | NG | |||||||
| Meduri et al[ | USA | M | 63 | 28 | 44/47 | 50.1±15.3 | 53.2±15.3 | Infusion of Me 1 mg/(kg·d) | Early severe ARDS | Up to 28 | 15/63 | 12/28 | 16.5±10.1 | 8.7±10.2 | 27/63 | 16/28 |
| Meduri et al[ | USA | M | 16 | 8 | 15/9 | 47.0±39.0 | 51.0±6.6 | Intravenous pushing Me 2 mg/(kg·d) | Unresolving ARDS | Up to 32 | 2/16 | 5/8 | NA | NA | 12/16 | 6/8 |
| Rezk et al[ | Egypt | M | 18 | 9 | 4/23 | NA | NA | Infusion of Me 1 mg/(kg·d) | Early ARDS | Up to 28 | 0/18 | 3/9 | NA | NA | NA | NA |
| Villar et al[ | Spain | M | 139 | 138 | 86/191 | 56.0±14.0 | 58.0±15.0 | Intravenously receiving Dex 20 mg/d | Early ARDS | Up to 10 | 29/139 | 50/138 | 12.3±9.9 | 7.5±9.0 | 33/139 | 35/138 |
| Tongyoo et al[ | Thailand | S | 98 | 99 | 96/101 | 64.5±17.3 | 64.3±16.0 | Intravenous bolus Hy 200 mg/d | Early ARDS | 7 | 22/98 | 27/99 | 12.0±9.7 | 9.7±10.0 | 34/98 | 41/99 |
| Annane et al[ | France | M | 85 | 92 | NA | NA | NA | Hy 200 mg/d and Flu 50 μg | Early ARDS | 7 | 54/85 | 67/92 | 4.9±8.4 | 3.1±6.9 | 12/85 | 12/92 |
| Steinberg et al[ | USA | M | 89 | 91 | 82/98 | 49.0±19.0 | 49.2±16.5 | Intravenously receivng Me 2 mg/(kg·d) | Unresolving ARDS | Up to 25 | 26/89 | 26/91 | 11.2±9.4 | 6.8±8.5 | 25/89 | 43/91 |
| Liu et al[ | China | S | 12 | 14 | 7/19 | 69.8±14.9 | 55.9±15.3 | Intravenous bolus Hy 300 mg/d | Early ARDS | 7 | 3/12 | 6/14 | 13.9±11.3 | 12.8±11.3 | 3/12 | 2/14 |

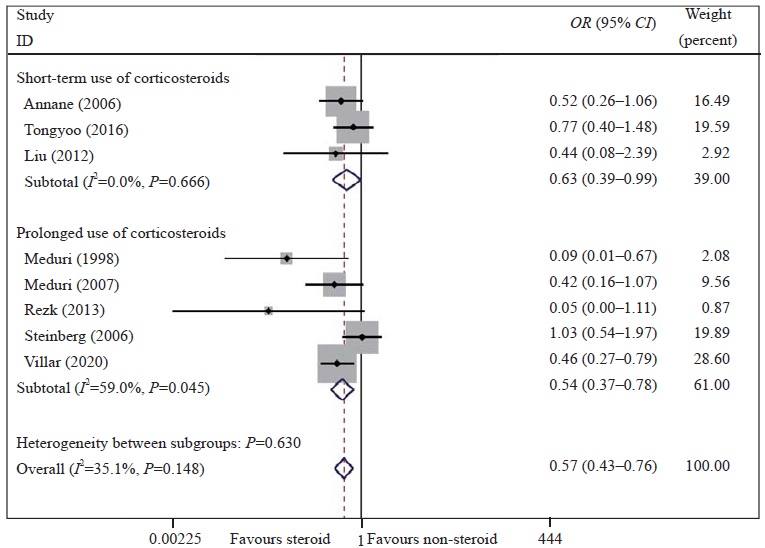
Figure 1.
Meta-analysis of overall pooled and subgroup OR with 95% CI across RCTs for the primary outcomes in patients with ARDS. Forest plot showing the significance of the relationship between the use of low-dose corticosteroids and mortality in patients with early and unresolving ARDS according to the fixed effects model; RCTs: randomized controlled trials; OR: odds ratio; CI: confidence interval; ARDS: acute respiratory distress syndrome.


Figure 2.
Meta-analysis of overall pooled and subgroup OR with 95% CI across RCTs for the primary outcomes in patients with ARDS. Forest plot showing the significance of the relationships between the prolonged use and short-term use of low-dose corticosteroids and mortality in ARDS patients according to the fixed effects model; RCTs: randomized controlled trials; OR: odds ratio; CI: confidence interval; ARDS: acute respiratory distress syndrome.
| 1 |
ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012; 307(23):2526-33.
doi: 10.1001/jama.2012.5669 pmid: 22797452 |
| 2 |
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016; 315(8):788-800.
doi: 10.1001/jama.2016.0291 |
| 3 |
Bein T, Grasso S, Moerer O, Quintel M, Guerin C, Deja M, et al. The standard of care of patients with ARDS: ventilatory settings and rescue therapies for refractory hypoxemia. Intensive Care Med. 2016; 42(5):699-711.
doi: 10.1007/s00134-016-4325-4 |
| 4 |
Fan YW, Jiang SW, Chen JM, Wang HQ, Liu D, Pan SM, et al. A pulmonary source of infection in patients with sepsis-associated acute kidney injury leads to a worse outcome and poor recovery of kidney function. World J Emerg Med. 2020; 11(1):18-26.
doi: 10.5847/wjem.j.1920-8642.2020.01.003 |
| 5 |
Wan YD, Sun TW, Liu ZQ, Zhang SG, Wang LX, Kan QC. Efficacy and safety of corticosteroids for community-acquired pneumonia: a systematic review and meta-analysis. Chest. 2016; 149(1):209-19.
doi: 10.1378/chest.15-1733 |
| 6 |
Fang F, Zhang Y, Tang J, Lunsford LD, Li T, Tang R, et al. Association of corticosteroid treatment with outcomes in adult patients with sepsis: a systematic review and meta-analysis. JAMA Intern Med. 2019; 179(2):213-23.
doi: 10.1001/jamainternmed.2018.5849 pmid: 30575845 |
| 7 |
Song LC, Chen XX, Meng JG, Hu M, Huan JB, Wu J, et al. Effects of different corticosteroid doses and durations on smoke inhalation-induced acute lung injury and pulmonary fibrosis in the rat. Int Immunopharmacol. 2019; 71:392-403.
doi: 10.1016/j.intimp.2019.03.051 |
| 8 |
Yu Z, Ouyang JP, Li YP. Dexamethasone attenuated endotoxin-induced acute lung injury through inhibiting expression of inducible nitric oxide synthase. Clin Hemorheol Microcirc. 2009; 41(2):117-25.
doi: 10.3233/CH-2009-1162 |
| 9 |
Thompson BT. Corticosteroids for ARDS. Minerva Anestesiol. 2010; 76(6):441-7.
pmid: 20473257 |
| 10 |
Wiegers GJ, Reul JMHM. Induction of cytokine receptors by glucocorticoids: functional and pathological significance. Trends Pharmacol Sci. 1998; 19(8):317-21.
pmid: 9745359 |
| 11 |
Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, et al. Methylprednisolone infusion in early severe ARDS: results of a randomized controlled trial. Chest. 2007; 131(4):954-63.
doi: 10.1378/chest.06-2100 |
| 12 |
Meduri GU, Headley AS, Golden E, Carson SJ, Umberger RA, Kelso T, et al. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1998; 280(2):159-65.
doi: 10.1001/jama.280.2.159 |
| 13 |
Rezk NA, Ibrahim AM. Effects of methyl prednisolone in early ARDS. Egyptian Journal of Chest Diseases and Tuberculosis. 2013; 62(1):167-72.
doi: 10.1016/j.ejcdt.2013.02.013 |
| 14 |
Villar J, Ferrando C, Martínez D, Ambrós A, Muñoz T, Soler JA, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020; 8(3):267-76.
doi: S2213-2600(19)30417-5 pmid: 32043986 |
| 15 |
Tongyoo S, Permpikul C, Mongkolpun W, Vattanavanit V, Udompanturak S, Kocak M, et al. Hydrocortisone treatment in early sepsis-associated acute respiratory distress syndrome: results of a randomized controlled trial. Crit Care. 2016; 20(1):329.
pmid: 27741949 |
| 16 |
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Int J Surg. 2010; 8(5):336-41.
doi: 10.1016/j.ijsu.2010.02.007 |
| 17 |
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ, et al. What is “quality of evidence” and why is it important to clinicians? BMJ. 2008; 336(7651):995-8.
doi: 10.1136/bmj.39490.551019.BE |
| 18 |
Chou R, Fu R, Carson S, Saha S, Helfand M. Methodological shortcomings predicted lower harm estimates in one of two sets of studies of clinical interventions. J Clin Epidemiol. 2007; 60(1):18-28.
doi: 10.1016/j.jclinepi.2006.02.021 |
| 19 | Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analyses. Available at: www.ohri.ca/programs/clinical_epidemiology/oxford.asp. |
| 20 |
Wetterslev J, Jakobsen JC, Gluud C. Trial sequential analysis in systematic reviews with meta-analysis. BMC Med Res Methodol. 2017; 17(1):39.
doi: 10.1186/s12874-017-0315-7 pmid: 28264661 |
| 21 |
Annane D, Sebille V, Bellissant E. Effect of low doses of corticosteroids in septic shock patients with or without early acute respiratory distress syndrome. Crit Care Med. 2006; 34(1):22-30.
doi: 10.1097/01.CCM.0000194723.78632.62 |
| 22 |
Steinberg KP, Hudson LD, Goodman RB, Hough CL, Lanken PN, Hyzy R, et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med. 2006; 354(16):1671-84.
doi: 10.1056/NEJMoa051693 |
| 23 | Liu L, Li J, Huang YZ, Liu SQ, Yang CS, Guo FM, et al. The effect of stress dose glucocorticoid on patients with acute respiratory distress syndrome combined with critical illness-related corticosteroid insufficiency. Zhonghua Nei Ke Za Zhi. 2012; 51(8):599-603. |
| 24 |
Keel JB, Hauser M, Stocker R, Baumann PC, Speich R. Established acute respiratory distress syndrome: benefit of corticosteroid rescue therapy. Respiration. 1998; 65(4):258-64.
pmid: 9730790 |
| 25 |
Lee HS, Lee JM, Kim MS, Kim HY, Hwangbo B, Zo JI. Low-dose steroid therapy at an early phase of postoperative acute respiratory distress syndrome. Ann Thorac Surg. 2005; 79(2):405-10.
doi: 10.1016/j.athoracsur.2004.07.079 |
| 26 |
Seam N, Meduri GU, Wang H, Nylen ES, Sun J, Schultz MJ, et al. Effects of methylprednisolone infusion on markers of inflammation, coagulation, and angiogenesis in early acute respiratory distress syndrome. Crit Care Med. 2012; 40(2):495-501.
doi: 10.1097/CCM.0b013e318232da5e |
| 27 |
Varpula T, Pettila V, Rintala E, Takkunen O, Valtonen V. Late steroid therapy in primary acute lung injury. Intensive Care Med. 2000; 26(5):526-31.
doi: 10.1007/s001340051199 |
| 28 |
Zhao JN, Liu Y, Li HC. Corticosteroids in treatment of aspiration-related acute respiratory distress syndrome: results of a retrospective cohort study. BMC Pulm Med. 2016; 16:29.
doi: 10.1186/s12890-016-0194-4 |
| 29 |
Baek MS, Lee Y, Hong SB, Lim CM, Koh Y, Huh JW. Effect of corticosteroid therapy in the early phase of acute respiratory distress syndrome: a propensity-matched cohort study. Korean J Intern Med. 2021; 36(1):145-53.
doi: 10.3904/kjim.2019.153 |
| 30 |
Chen LP, Chen JH, Chen Y, Wu C, Yang XH. Efficacy and safety of glucocorticoids in the treatment of community-acquired pneumonia: a meta-analysis of randomized controlled trials. World J Emerg Med. 2015; 6(3):172-8.
doi: 10.5847/wjem.j.1920-8642.2015.03.002 |
| 31 |
Matthay MA, Zemans RL, Zimmerman GA, Arabi YM, Beitler JR, Mercat A, et al. Acute respiratory distress syndrome. Nat Rev Dis Primers. 2019; 5(1):18.
doi: 10.1038/s41572-019-0069-0 |
| 32 |
Meduri GU, Eltorky MA. Understanding ARDS-associated fibroproliferation. Intensive Care Med. 2015; 41(3):517-20.
doi: 10.1007/s00134-014-3613-0 |
| 33 |
Meduri GU, Chinn AJ, Leeper KV, Wunderink RG, Tolley E, Winer-Muram HT, et al. Corticosteroid rescue treatment of progressive fibroproliferation in late ARDS. Chest. 1994; 105(5):1516-27.
pmid: 8181346 |
| 34 |
Kellum JA, Kong L, Fink MP, Weissfeld LA, Yealy DM, Pinsky MR, et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch Intern Med. 2007; 167(15):1655-63.
pmid: 17698689 |
| 35 |
Lekkou A, Karakantza M, Mouzaki A, Kalfarentzos F, Gogos CA. Cytokine production and monocyte HLA-DR expression as predictors of outcome for patients with community-acquired severe infections. Clin Diagn Lab Immunol. 2004; 11(1):161-7.
pmid: 14715564 |
| 36 |
Meduri GU, Yates CR. Systemic inflammation-associated glucocorticoid resistance and outcome of ARDS. Ann N Y Acad Sci. 2004; 1024:24-53.
doi: 10.1196/annals.1321.004 |
| [1] | Wen Gao, Yu-ping Zhang, Jing-fen Jin. Poor outcomes of delirium in the intensive care units are amplified by increasing age: A retrospective cohort study [J]. World Journal of Emergency Medicine, 2021, 12(2): 117-123. |
| [2] | Xin Lu, Wei Han, Yan-xia Gao, Shi-gong Guo, Shi-yuan Yu, Xue-zhong Yu, Hua-dong Zhu, Yi Li. Efficacy and safety of corticosteroids in immunocompetent patients with septic shock [J]. World Journal of Emergency Medicine, 2021, 12(2): 124-130. |
| [3] | Hao-tian Chen, Jian-feng Xu, Xiao-xia Huang, Ni-ya Zhou, Yong-kui Wang, Yue Mao. Blood eosinophils and mortality in patients with acute respiratory distress syndrome: A propensity score matching analysis [J]. World Journal of Emergency Medicine, 2021, 12(2): 131-136. |
| [4] | Wei Guo, Lin-yu Ran, Ji-hong Zhu, Qing-gang Ge, Zhe Du, Fei-long Wang, Wei-bo Gao, Tian-bing Wang. Identifying critically ill patients at risk of death from coronavirus disease [J]. World Journal of Emergency Medicine, 2021, 12(1): 18-23. |
| [5] | Yi Han, Su-cheng Mu, Jian-li Wang, Wei Wei, Ming Zhu, Shi-lin Du, Min Min, Yun-jie Xu, Zhen-ju Song, Chao-yang Tong. MicroRNA-145 plays a role in mitochondrial dysfunction in alveolar epithelial cells in lipopolysaccharide-induced acute respiratory distress syndrome [J]. World Journal of Emergency Medicine, 2021, 12(1): 54-60. |
| [6] | Yu-ming Wang, Yan-jun Zheng, Ying Chen, Yun-chuan Huang, Wei-wei Chen, Ran Ji, Li-li Xu, Zhi-tao Yang, Hui-qiu Sheng, Hong-ping Qu, En-qiang Mao, Er-zhen Chen. Effects of fluid balance on prognosis of acute respiratory distress syndrome patients secondary to sepsis [J]. World Journal of Emergency Medicine, 2020, 11(4): 216-222. |
| [7] | Rui-xue Sun, Priscilla Song, Joseph Walline, He Wang, Ying-chun Xu, Hua-dong Zhu, Xue-zhong Yu, Jun Xu. Morbidity and mortality risk factors in emergency department patients with Acinetobacter baumannii bacteremia [J]. World Journal of Emergency Medicine, 2020, 11(3): 164-168. |
| [8] | Shao-hua Liu, Huo-yan Liang, Hong-yi Li, Xian-fei Ding, Tong-wen Sun, Jing Wang. Effect of low high-density lipoprotein levels on mortality of septic patients: A systematic review and meta-analysis of cohort studies [J]. World Journal of Emergency Medicine, 2020, 11(2): 109-116. |
| [9] | Wei He, Yue-yang You, Kai Sun, Chen Xie, Yue Ming, Li-na Yu, Feng-jiang Zhang, Min Yan. Admission delay is associated with worse surgical outcomes for elderly hip fracture patients: A retrospective observational study [J]. World Journal of Emergency Medicine, 2020, 11(1): 27-32. |
| [10] | Shi-yuan Yu, Yan-xia Gao, Joseph Walline, Xin Lu, Li-na Zhao, Yuan-xu Huang, Jiang Tao, An-yong Yu, Na Ta, Ren-ju Xiao, Yi Li. Role of penehyclidine in acute organophosphorus pesticide poisoning [J]. World Journal of Emergency Medicine, 2020, 11(1): 37-47. |
| [11] | Chang Pan, Xiao-ran Huang, Jiao-jiao Pang, Kai Cheng, Feng Xu, Yu-guo Chen. Trends in mortality of emergency departments patients in China [J]. World Journal of Emergency Medicine, 2019, 10(3): 152-155. |
| [12] | Hui Xie, Zhi-gang Zhou, Wei Jin, Cheng-bin Yuan, Jiang Du, Jian Lu, Rui-lan Wang. Ventilator management for acute respiratory distress syndrome associated with avian influenza A (H7N9) virus infection: A case series [J]. World Journal of Emergency Medicine, 2018, 9(2): 118-124. |
| [13] | Yuzeng Shen, Yee Chien Tay, Edward Wee Kwan Teo, Nan Liu, Shao Wei Lam, Marcus Eng Hock Ong. Association between the elderly frequent attender to the emergency department and 30-day mortality: A retrospective study over 10 years [J]. World Journal of Emergency Medicine, 2018, 9(1): 20-25. |
| [14] | Kasim Turgut, Mehmet Ediz Sarihan, Cemil Colak, Taner Güven, Ali Gür, Sükrü Gürbüz. Falls from height: A retrospective analysis [J]. World Journal of Emergency Medicine, 2018, 9(1): 46-50. |
| [15] | Youichi Yanagawa, Kouhei Ishikawa, Kei Jitsuiki, Toshihiko Yoshizawa, Yasumasa Oode, Kazuhiko Omori, Hiromichi Ohsaka. Fibrinogen degradation product levels on arrival for trauma patients requiring a transfusion even without head injury [J]. World Journal of Emergency Medicine, 2017, 8(2): 106-109. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
