World Journal of Emergency Medicine ›› 2015, Vol. 6 ›› Issue (4): 277-282.doi: 10.5847/wjem.j.1920-8642.2015.04.005
• Original Articles • Previous Articles Next Articles
Andrew Fu Wah Ho1( ), Pin Pin Pek2, Stephanie Fook-Chong3, Ting Hway Wong4, Yih Yng Ng5, Aaron Sung Lung Wong6, Marcus Eng Hock Ong2
), Pin Pin Pek2, Stephanie Fook-Chong3, Ting Hway Wong4, Yih Yng Ng5, Aaron Sung Lung Wong6, Marcus Eng Hock Ong2
Received:2015-03-28
Accepted:2015-09-10
Online:2015-12-15
Published:2015-12-15
Contact:
Andrew Fu Wah Ho
E-mail:sophronesis@gmail.com
Andrew Fu Wah Ho, Pin Pin Pek, Stephanie Fook-Chong, Ting Hway Wong, Yih Yng Ng, Aaron Sung Lung Wong, Marcus Eng Hock Ong. Prehospital system delay in patients with ST-segment elevation myocardial infarction in Singapore[J]. World Journal of Emergency Medicine, 2015, 6(4): 277-282.
Add to citation manager EndNote|Ris|BibTeX
URL: http://wjem.com.cn//EN/10.5847/wjem.j.1920-8642.2015.04.005
Figure 1.
Components of delay in ST-segment elevation myocardial infarction and recommended time intervals by 2012 European Society of Cardiology (ESC) guideline and 2013 American College of Cardiology Foundation/American Heart Association (ACC/AHA). PCI: percutaneous coronary intervention; EMS: emergency medical services; ESC: European Society of Cardiology; ACC/AHA: American College of Cardiology Foundation/American Heart Association
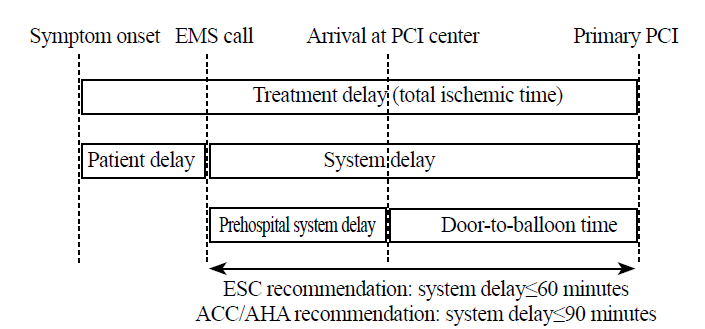
Table 1
Correlates of pre-hospital system delay (first medical contact to door time)
| Variables | All (n=52) | FC2D<35.5 minutes (n=26) | FC2D>35.5 minutes (n=26) | P value |
|---|---|---|---|---|
| Demographics | ||||
| Age, median (range), years | 56.0 (36.0-79.0) | 54.0 (41.0-74.0) | 58.0 (36.0-79.0) | 0.213 |
| Gender (n, %) | 0.714 | |||
| Male | 43 (82.7) | 21 (80.8) | 22 (84.6) | |
| Female | 9 (17.3) | 5 (19.2) | 4 (15.4) | |
| Race (n, %) | 0.629 | |||
| Chinese | 31 (59.6) | 17 (65.4) | 14 (53.8) | |
| Malay | 9 (17.3) | 5 (19.2) | 4 (15.4) | |
| Indian | 9 (17.3) | 6 (23.1) | 3 (11.5) | |
| Others | 3 (5.8) | 1 (3.8) | 2 (7.7) | |
| Presenting circumstances | ||||
| Chest pain/discomfort (n, %) | 45 (86.5) | 23 (88.5) | 22 (84.6) | 0.685 |
| Incident location (n, %) | 0.780 | |||
| Residential | 29 (55.8) | 14 (53.8) | 15 (57.7) | |
| Non-residential | 23 (44.2) | 12 (46.2) | 11 (42.3) | |
| Pain score, mean | 4.27 | 4.44 | 4.12 | 0.834 |
| Glasgow coma scale score, mean | 14.82 | 14.88 | 14.76 | 0.332 |
| Transport conditions (n, %) | ||||
| Weather conditions | 0.720 | |||
| Sunny-fine | 46 (88.5) | 24 (92.3) | 22 (84.6) | |
| Light rain | 2 (3.8) | 1 (3.8) | 1 (3.8) | |
| Heavy rain | 1 (1.9) | 0 (0) | 1 (3.8) | |
| Windy | 2 (3.8) | 1 (3.8) | 1 (3.8) | |
| Traffic conditions | 0.871 | |||
| Light | 4 (8.0) | 2 (8.3) | 2 (7.7) | |
| Moderate | 43 (86.0) | 21 (87.5) | 22 (84.6) | |
| Heavy | 3 (6.0) | 2 (7.7) | 1 (4.2) | |
| Prehospital interventions by paramedic (n, %) | ||||
| GTN (sublingual or transdermal) | 28 (53.8) | 13 (50.0) | 15 (57.7) | 0.578 |
| Aspirin | 7 (13.5) | 3 (11.5) | 4 (15.4) | 0.685 |
| Process of care intervals, median (range), minute | ||||
| Call-to-dispatch time | 2.48 (1.47-16.55) | 2.04 (1.60-5.02) | 2.92 (1.47-16.55) | 0.023 |
| Dispatch-to-arrival-at-patient time | 8.067 (1.30-22.13) | 5.75 (3.58-12.75) | 9.37 (1.30-22.13) | <0.01 |
| Arrival-at-patient-to-leaving patient time | 13.12 (3.12-32.2) | 10.78 (3.12-19.20) | 14.37 (8.07-32.22) | <0.01 |
| Leaving-patient-to-door time | 9.90 (1.62-32.92) | 7.80 (1.62-17.45) | 12.88 (5.25-32.92) | 0.016 |
| Symptom-to-balloon time | 217 (96.0-3038.0) | 222.0 (104.0-3038.0) | 189.0 (96.0-736.0) | 0.104 |
| Door-to-balloon time | 92.0 (62.0-177.0) | 91.0 (62.0-160.0) | 94.0 (65.0-177.0) | 0.331 |
| 1 | Health Facts Singapore 2012. Ministry of Health Singapore. http://www.moh.gov.sg/content/moh_web/home/statistics/Health_Facts_Singapore/Principal_Causes_of_Death.html. Accessed November 27, 2013. |
| 2 | The top 10 causes of death. World Health Organization Fact Sheets. http://www.who.int/mediacentre/factsheets/fs310/en/index3.html. Accessed November 27, 2013. |
| 3 | Reimer KA, Jennings RB. The "wavefront phenomenon" of myocardial ischemic cell death. II. Transmural progression of necrosis within the framework of ischemic bed size (myocardium at risk) and collateral flow. Lab Invest 1979; 40:633-644. |
| 4 | Gersh BJ, Stone GW, White HD, Holmes DR. Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future? JAMA 2005; 293:979-986. |
| 5 | Shiomi H, Nakagawa Y, Morimoto T, Furukawa Y, Nakano A, Shirai S, et al. Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ 2012; 3257:1-14. |
| 6 |
Anderson JL, Karagounis La, Califf RM. Meta-analysis of five reported studies on the relation of early coronary patency grades with mortality and outcomes after acute myocardial infarction. Am J Cardiol 1996; 78:1-8.
pmid: 8712096 |
| 7 |
De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 2004; 109:1223-1225.
pmid: 15007008 |
| 8 |
Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010; 304:763-771.
pmid: 20716739 |
| 9 | Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012; 33:2569-2619. |
| 10 |
O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013; 127:e362-425.
pmid: 23247304 |
| 11 | Srimahachota S, Kanjanavanit R, Boonyaratavej S, Boonsom W, Veerakul G, Tresukosol D, et al. Demographic, management practices and in-hospital outcomes of Thai Acute Coronary Syndrome Registry (TACSR): the difference from the Western world. J Med Assoc Thai 2007; 90 Suppl 1: 1-11. |
| 12 | Song L, Yan H, Hu D, Yang J, Sun Y. Pre-hospital care-seeking in patients with acute myocardial infarction and subsequent quality of care in Beijing. Chin Med J (Engl) 2010; 123:664-669. |
| 13 | Ho AFW, Fook-Chong S, Pek PP, Ng YY, Wong ASL, Ong MEH. Prehospital presentation of patients with ST-segment elevation myocardial infarction in Singapore. Int J Cardiol 2013; 168:4273-4276. |
| 14 |
Tan LL, Wong HB, Poh CL, Chan MY, Seow SC, Yeo TC, et al. Utilisation of emergency medical service among Singapore patients presenting with ST-segment elevation myocardial infarction: prevalence and impact on ischaemic time. Intern Med J 2011; 41:809-814.
pmid: 20546061 |
| 15 | Statistics Singapore. Department of Statistics Singapore. http://www.singstat.gov.sg/statistics/latest_data.html#14. Accessed November 27, 2013. |
| 16 |
Shin SD, Ong MEH, Tanaka H, Ma MH, Nishiuchi T, Alsakaf O, et al. Comparison of emergency medical services systems across Pan-Asian countries: a Web-based survey. Prehosp Emerg Care 2012; 16:477-496.
pmid: 22861161 |
| 17 |
Ong MEH, Chan YH, Anantharaman V, Lau ST, Lim SH, Seldrup J. Cardiac arrest and resuscitation epidemiology in Singapore (CARE I study). Prehosp Emerg Care 2003; 7:427-433.
pmid: 14582091 |
| 18 |
Ong MEH, Wong ASL, Seet CM, Teo SG, Lim BL, Ong PJ, et al. Nationwide improvement of door-to-balloon times in patients with acute ST-segment elevation myocardial infarction requiring primary percutaneous coronary intervention with out-of-hospital 12-lead ECG recording and transmission. Ann Emerg Med 2013; 61:339-347.
doi: 10.1016/j.annemergmed.2012.08.020 pmid: 23021348 |
| 19 |
Huber K, De Caterina R, Kristensen SD, Verheugt FW, Montalescot G, Maestro LB, et al. Pre-hospital reperfusion therapy: a strategy to improve therapeutic outcome in patients with ST-elevation myocardial infarction. Eur Heart J 2005; 26:2063-2074.
doi: 10.1093/eurheartj/ehi413 pmid: 16055497 |
| [1] | Tian Xu, Ya Li, Li-ding Zhao, Guo-sheng Fu, Wen-bin Zhang. Predictors of recurrent angina in patients with no need for secondary revascularization [J]. World Journal of Emergency Medicine, 2021, 12(1): 42-47. |
| [2] | Guo-xiong Chen, Hong-na Wang, Jin-lin Zou, Xiao-xu Yuan. Effects of intracoronary injection of nicorandil and tirofiban on myocardial perfusion and short-term prognosis in elderly patients with acute ST-segment elevation myocardial infarction after emergency PCI [J]. World Journal of Emergency Medicine, 2020, 11(3): 157-163. |
| [3] | Jun Jiang, Nai-liang Tian, Han-bin Cui, Chang-ling Li, Xian-bao Liu, Liang Dong, Yong Sun, Xiao-min Chen, Shao-liang Chen, Bo Xu, Jian-an Wang. Post-dilatation improves stent apposition in patients with ST-segment elevation myocardial infarction receiving primary percutaneous intervention: A multicenter, randomized controlled trial using optical coherence tomography [J]. World Journal of Emergency Medicine, 2020, 11(2): 87-92. |
| [4] | Hong-yi Wu, Ju-ying Qian, Qi-bing Wang, Jun-bo Ge. An unexpected electrocardiogram sign of subacute left ventricular free wall rupture: Its early awareness may be lifesaving [J]. World Journal of Emergency Medicine, 2020, 11(2): 117-119. |
| [5] | Wei He, Yue-yang You, Kai Sun, Chen Xie, Yue Ming, Li-na Yu, Feng-jiang Zhang, Min Yan. Admission delay is associated with worse surgical outcomes for elderly hip fracture patients: A retrospective observational study [J]. World Journal of Emergency Medicine, 2020, 11(1): 27-32. |
| [6] | Colin A. Meghoo, Stanislav Gaievskyi, Oleksandr Linchevskyy, Bindhu Oommen, Kateryna Stetsenko. Prehospital response to respiratory distress by the public ambulance system in a Ukrainian city [J]. World Journal of Emergency Medicine, 2019, 10(1): 42-45. |
| [7] | Linda Chokotho, Wakisa Mulwafu, Isaac Singini, Yasin Njalale, Kathryn H. Jacobsen. Improving hospital-based trauma care for road traffic injuries in Malawi [J]. World Journal of Emergency Medicine, 2017, 8(2): 85-90. |
| [8] | Li-ming Li, Wen-bo Cai, Qin Ye, Jian-min Liu, Xin Li, Xiao-xing Liao. Comparison of plasma microRNA-1 and cardiac troponin T in early diagnosis of patients with acute myocardial infarction [J]. World Journal of Emergency Medicine, 2014, 5(3): 182-186. |
| [9] | Hua Zhou, Xiao-yan He, Shao-wei Zhuang, Juan Wang, Yan Lai, Wei-gang Qi, Yi-an Yao, Xue-bo Liu. Clinical and procedural predictors of no-reflow in patients with acute myocardial infarction after primary percutaneous coronary intervention [J]. World Journal of Emergency Medicine, 2014, 5(2): 96-102. |
| [10] | Ya Zhong, Ping Cao, Chuan-feng Tong, Xia Li. Effects of ramipril on ventricular arrhythmia after myocardial infarction in rabbits [J]. World Journal of Emergency Medicine, 2014, 5(2): 135-138. |
| [11] | Li-li Ji, Xiao-feng Long, Hui Tian, Yu-fei Liu. Effect of transplantation of bone marrow stem cells on myocardial infarction size in a rabbit model [J]. World Journal of Emergency Medicine, 2013, 4(4): 304-310. |
| [12] | Özlem Köksal, Fatma Özdemir, Erol Armağan, Nuran Öner, Pınar Çinar Sert, Deniz Sigirli. Is routine pregnancy test necessary in women of reproductive age admitted to the emergency department? [J]. World Journal of Emergency Medicine, 2013, 4(3): 175-178. |
| [13] | Chun-tao Wu, Zhong-hua Wang, Zhu-qin Li, Lan-feng Wang. Effect of spironolactone on cardiac remodeling after acute myocardial infarction [J]. World Journal of Emergency Medicine, 2013, 4(1): 48-53. |
| [14] | Yan Chen, Wei Yang, Gan-nan Wang, Jun Li, Xiao-rong Li, Jian Zhang, Wei Yuan, Dao-wu Wang, Jin-song Zhang, Ke-jiang Cao. Circulating microRNAs, novel biomarkers of acute myocardial infarction: a systemic review [J]. World Journal of Emergency Medicine, 2012, 3(4): 257-260. |
| [15] | Li Chen, Xian-lun Li, Wei Qiao, Zhou Ying, Yan-li Qin, Yong Wang, Yu-jie Zeng, Yuan-nan Ke. Serum uric acid in patients with acute ST-elevation myocardial infarction [J]. World Journal of Emergency Medicine, 2012, 3(1): 35-39. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||
